If you’re caring for a parent, partner, or child, you’ve likely felt the quiet exhaustion that seeps into everything—the way simple decisions get heavier, the way nights blur. Meditation for caregiver burnout is a practical, science-backed way to soften stress, steady your mind, and rebuild emotional reserves. Ten minutes is enough. Ten minutes most days is better. Of all coping tools, meditation is the most portable—and perhaps the most forgiving. News outlets like The Guardian have chronicled the invisible load many families carried in 2020 and beyond; Harvard Health has, for years, noted mindfulness can ease stress and modestly improve sleep. That lines up with what caregivers report on the ground.
Table of Contents
- Why caregivers burn out (and why this matters)
- The science behind meditation for caregiver burnout
- How to start meditation for caregiver burnout: a 10-minute plan
- Micro-moments for busy days
- Tools that make it easier
- Overcoming common obstacles
- Measure progress so you can see it working
- When meditation isn’t enough
- A compassionate reminder
- Summary
- References
Why caregivers burn out (and why this matters)
- There are 53 million family caregivers in the U.S., and 61% are women (AARP/NAC, 2020).
- Up to 40–70% report clinically significant symptoms of depression, and anxiety is common (Family Caregiver Alliance).
- Nearly 1 in 4 caregivers rates their health as fair/poor; high caregiver stress predicts worse immune function and more chronic illness risk over time (AARP/NAC, 2020).
Caregiver burnout isn’t a personal failure. It’s a nervous system pushed past its capacity by chronic demands, sleep disruption, and emotional load. If anything, our systems undercount the strain—and the hours—families quietly absorb.
The science behind meditation for caregiver burnout
Meditation trains attention and emotion regulation. It downshifts the stress response (HPA axis), reduces amygdala reactivity, and enhances prefrontal control—the brain’s “brakes.” Back in 2014, a large JAMA Internal Medicine review helped put mindfulness on the clinical map; since then, replication in frontline workers and family caregivers has been steady.
- A JAMA Internal Medicine meta-analysis of 47 trials found mindfulness programs produced moderate reductions in anxiety and depression comparable to antidepressants for some outcomes (Goyal et al., 2014). Link
- In healthcare workers, mindfulness-based interventions reduce stress and burnout with small-to-moderate effects (Burton et al., 2017). Link
- For dementia caregivers, randomized trials show mindfulness-based stress reduction improves perceived stress, depression, and sleep versus usual care or psychoeducation (Whitebird et al., 2013; Brown et al., 2016). Whitebird et al. | Brown et al.
Bottom line: mindfulness meditation directly targets caregiver stress and improves emotional well-being—key levers in preventing burnout. Frankly, the evidence is strong enough to act on between appointments.
How to start meditation for caregiver burnout: a 10-minute plan
You don’t need silence or a cushion. You need structure you can keep. In my view, structure beats willpower every time.
Morning (5 minutes): Anchoring breath
- Sit, feet on floor.
- Inhale through the nose for 4, exhale for 6—longer exhales nudge the body toward calm.
- When thoughts intrude (“Did I refill meds?”), silently note “thinking,” and return to breath.
- If fatigued, keep eyes open and soften your gaze.
Midday (3 minutes): Mindful check-in
- 60 sec body scan: crown to toes, notice tension; unclench jaw, drop shoulders.
- 60 sec breath: hand on chest or belly, feel rise/fall.
- 60 sec intention: “Today I will meet stress with one slow breath.” This primes behavior via implementation intentions.
Evening (10 minutes, optional): Loving-kindness for both of you
- Picture yourself, then your care recipient.
- Silently repeat: “May I be safe. May I be strong. May I meet this moment with kindness.” Then replace “I” with their name.
- Loving-kindness meditation increases positive emotions and social connection (Fredrickson et al., 2008), a powerful buffer against caregiver burnout. Done regularly, this one practice can thaw a hard day.
Micro-moments for busy days
- Handwashing: 20 seconds of breath counting.
- Waiting on hold: soften shoulders, lengthen exhale.
- Bedtime: 1–3 minutes of body scan instead of scrolling.
- During difficult tasks: silently label feelings (“sadness,” “frustration”). Name it to tame it.
Tiny, repeated cues change behavior—I’m convinced these crumbs matter more than heroic bursts.
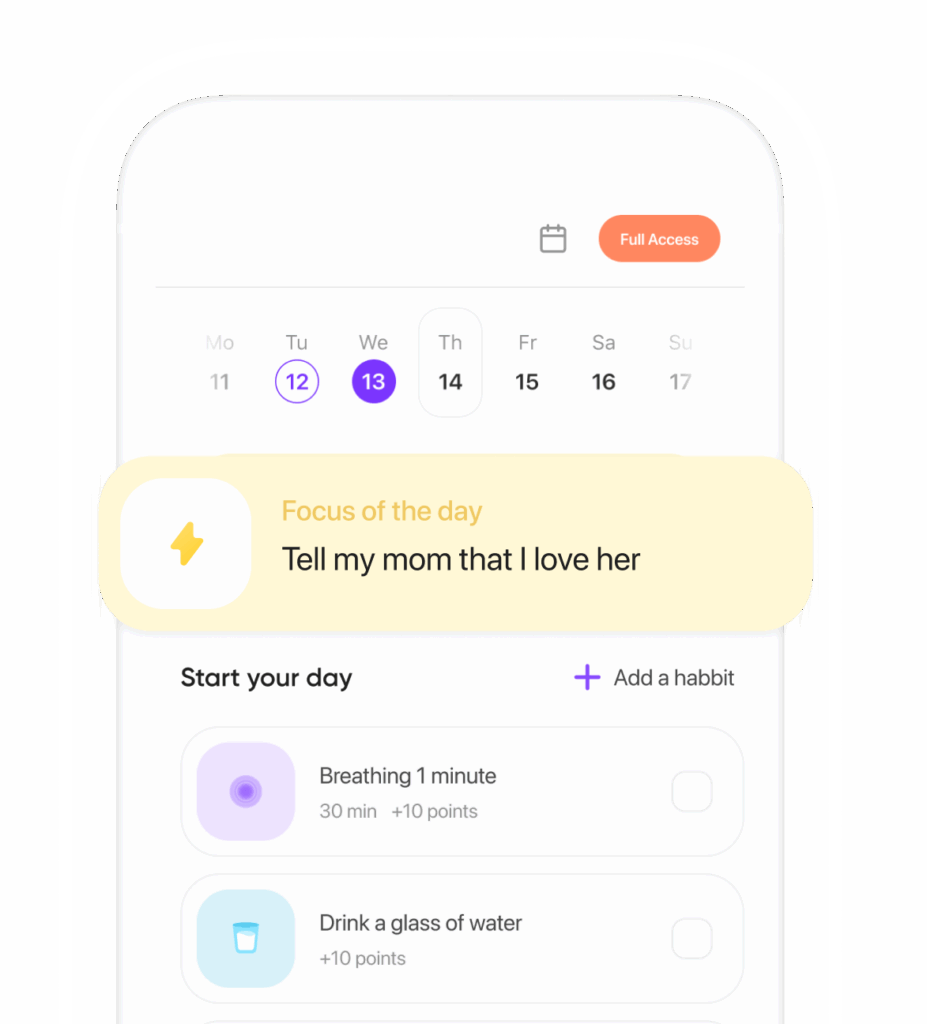
Tools that make it easier
- Free apps: UCLA Mindful, Healthy Minds Program, Smiling Mind.
- Reminders: pair practice with stable cues—first sip of coffee, car ignition, brushing teeth. Habit stacking beats willpower.
- Trackable wins: a sticky note habit streak, or a smartwatch prompt to breathe when heart rate spikes.
If you choose one tool, choose the one you’ll actually open. Simple wins—visible ones—keep the loop going.
Overcoming common obstacles
- “I’m too tired.” Do 2 minutes. Studies show even brief mindfulness bouts reduce state anxiety and improve attention. Consistency over intensity.
- “My mind won’t stop.” That’s normal. The rep is noticing you’ve wandered and returning—like a mental bicep curl.
- “I feel guilty taking time.” Reframe as care quality. Mindfulness improves empathy and reduces emotional exhaustion in caregivers and clinicians, which can enhance the care you provide (Burton et al., 2017).
Two minutes is still a practice. On hard weeks, that’s not a compromise; it’s a strategy.
Measure progress so you can see it working
- Every Sunday, rate 0–10: stress, sleep quality, patience, and one win.
- Use brief scales monthly: PSS-10 (Perceived Stress Scale) or the 12-item Zarit Burden Interview–Short Form.
- If you wear a tracker, watch resting heart rate trends; mind–body practices can modestly improve HRV over time.
Measuring isn’t cold; it’s humane. It lets you witness change that otherwise disappears into busy days.
When meditation isn’t enough
Meditation for caregiver burnout is one pillar, not the whole house. Add:
- Respite: ask your clinic about adult day programs or community respite grants.
- Skills: caregiver training can reduce behavioral stressors and boost confidence (AHRQ).
- Therapy: CBT or acceptance and commitment therapy help reframe unhelpful thoughts; many counties offer low-cost options.
- Crisis: if you feel unsafe or hopeless, call or text 988 (U.S.) for 24/7 support.
No single practice can carry the full weight—nor should it. A layered plan is kinder and more resilient.
A compassionate reminder
Start where you are. Ten imperfect minutes of mindfulness meditation a day can nudge your nervous system toward steadiness, lighten caregiver stress, and rebuild bandwidth. Some days you’ll manage three minutes… and that counts. Over weeks, meditation for caregiver burnout becomes less another task and more a way you move through the day—with clarity, warmth, and a little more room to breathe.
Summary
Meditation for caregiver burnout offers a realistic, evidence-based path to lower stress, better mood, and more resilient care. Use short daily practices—anchored breath, mindful check-ins, and loving-kindness—plus habit cues and simple tracking. Pair meditation with respite, skills, and support for strongest results. Bold, tiny steps compound into real relief. Start your 10-minute plan today—set a timer, breathe out longer, and give yourself the same care you give others.
References
- Goyal M, et al. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern Med. 2014. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1809754
- Burton A, et al. Mindfulness for health care professionals: Systematic review and meta-analysis. Mindfulness. 2017. https://link.springer.com/article/10.1007/s12671-017-0819-2
- Whitebird RR, et al. Mindfulness-based stress reduction for family caregivers of persons with dementia. Am J Geriatr Psychiatry. 2013. https://www.sciencedirect.com/science/article/abs/pii/S1064748112003423
- Brown KW, Coogle CL, Wegelin J. A pilot RCT of MBSR for caregivers of family members with dementia. Aging & Mental Health. 2016. https://www.tandfonline.com/doi/full/10.1080/13607863.2015.1065790
- AARP & National Alliance for Caregiving. Caregiving in the U.S. 2020. https://www.caregiving.org/caregiving-in-the-us-2020
- Family Caregiver Alliance. Caregiver mental health statistics. https://www.caregiver.org/resource/caregiver-health/
- Fredrickson BL, et al. Open hearts build lives: LKM increases positive emotions. J Pers Soc Psychol. 2008. https://psycnet.apa.org/record/2008-04342-003
- Agency for Healthcare Research and Quality (AHRQ). Caregiver interventions. https://effectivehealthcare.ahrq.gov/products/caregiver-interventions/research-protocol
Ready to transform your life? Install now ↴
Join 1.5M+ people using AI-powered app for better mental health, habits, and happiness. 90% of users report positive changes in 2 weeks.