If you or your partner lives with obsessive–compulsive disorder, the 7 Love Languages for OCD can offer a humane framework for care—firm, warm, and pointed toward recovery rather than ritual. OCD affects roughly 1–2% of adults each year and often shows up before 19 (NIMH). Therapy remains the backbone; at its core, exposure and response prevention (ERP) is the gold standard. But what happens between sessions—the everyday habits, the way you talk at 9 p.m. when anxiety spikes—often determines whether gains stick. I’ve seen that day-to-day care either fortifies treatment or quietly undermines it.
Quick evidence check: ERP and CBT have strong, consistent effects for OCD; the pre–post changes reported in meta-analyses are large and clinically meaningful. A 2013 review in Clinical Psychology Review spelled this out clearly, and nothing since has dethroned it. “Love languages,” by contrast, have mixed research support as a theory. Still, as a practical scaffold—something couples can use to cue supportive behavior and reduce accommodation—they’re useful. I’d argue pragmatic tools that help partners row in the same direction beat purist debates, most days.
What are the 7 Love Languages for OCD?
Here’s the set we’ll use—five classics plus two contemporary add-ons that fit modern life:
- Words of affirmation
- Quality time
- Acts of service
- Physical touch
- Receiving gifts
- Digital connection (texts/DMs)
- Shared experiences/play
Ground rules that keep the 7 Love Languages for OCD helpful, not harmful:
- Pair care with treatment goals. Wherever possible, match your support to the ERP/CBT plan on paper. It keeps love from becoming a loophole.
- Reduce accommodation. Partner accommodation (e.g., repeated reassurance, joining rituals) is common and linked to worse symptoms; replacing it with compassionate limits is associated with better outcomes. Hard, yes—vital, also yes.
- Agree on “reassurance boundaries.” Decide upfront when reassurance is supportive (once, brief) versus compulsive (repetitive, ritualistic). The line creeps; write it down.
- Practice consent and pacing. For triggers and exposures, move at an agreed therapeutic pace—planned discomfort, not surprises. In my view, repair is faster when the process feels fair.
How to use the 7 Love Languages for OCD in daily life
Words of affirmation
- Validate without feeding compulsions: “I see how hard this is, and I’m proud you’re resisting the urge.” Avoid answering the same “Are you sure?” on loop. Validation is a stance, not a ritual.
- Praise growth, not certainty: “You sat with uncertainty for 5 minutes—huge win.” Track effort and duration, not whether the fear vanished.
- ERP-aligned language: “We’re choosing uncertainty together.” Short, steady phrases can become anchors when the urge spikes. Personally, I think language that normalizes “maybe” is underrated.
Quality time
- Exposure buddy time: Join planned exposures—a short walk without rechecking locks; touching a “contaminated” doorknob—while declining post-exposure reassurance loops. Be present, not the safety signal.
- Ritual-free routines: Cook, watch a show, or walk the dog without accommodating hand-washing or checking. Use timers to hold boundaries: one wash, then dinner.
- Weekly check-in: Twenty minutes to review what helped, what slid into accommodation, and what adjusts next week. The Guardian reported during the 2020 lockdowns that couples who set regular check-ins navigated mental-health stress more effectively; I’ve found the same.
Acts of service
- Helpful, not enabling: Drive to therapy, help map an exposure ladder, set up a calming corner for post-exposure decompression—without assisting rituals. Support the work, not the workaround.
- Task segmentation: Break chores into exposure-friendly steps (e.g., load the dishwasher once, then stop). One clear step beats a vague promise.
- “One-and-done” help: Provide an answer once (“Yes, the stove is off”), then gently decline further reassurance. It’s kinder than indulging the loop.
Physical touch
- Co-regulation: Offer a hand hold or steadying hug before/after an exposure—not as a ritual in the anxiety peak. Touch as bookends, not a neutralizer.
- Touch as an uncertainty cue: “We can hold hands while we let the worry be there.” The message: comfort, while uncertainty stays.
- Boundaries with ROCD (relationship-themed OCD): If constant cuddling turns into a feelings-checking compulsion, set limits and schedule affectionate time instead. It may feel counterintuitive; it’s wiser.
Receiving gifts
- Therapy-aligned tools: A journal for exposure notes, a cozy blanket for decompression, a visual timer for response prevention. Practical beats splashy.
- Symbolic gifts of uncertainty: A small bracelet engraved “Maybe” or “I can handle not knowing” as a values reminder. Tiny, visible, steadying.
- Experience vouchers: A coffee date after an exposure—not a bribe, a values-based pairing of hard work with living. I’d take this over reassurance any day.
Digital connection
- Text templates that block reassurance loops: “I believe in your plan. You’ve got this,” rather than re-answering the same safety question. Signal confidence in the process.
- “One response” policy: Offer one supportive reply, then switch to value-focused topics. Boundaries are kinder than the endless scroll.
- Digital limits: Reduce symptom-checking searches together; use app blockers during high-vulnerability hours. In 2021, several clinics flagged late-night Googling as a frequent trigger—no surprise.
Shared experiences/play
- Micro-adventures with mild uncertainty: New café, spur-of-the-moment day trip, board game night—practice “good enough” decisions without over-research. Imperfect and done.
- Play as exposure: Try improv or low-stakes challenges that welcome mistakes. Laughter can teach the nervous system it’s safe to wobble.
- Values-first planning: Choose activities around personal values (creativity, service, connection), not OCD’s rules. In my opinion, values talk is the best compass in tough weeks.
A 3-step plan to implement the 7 Love Languages for OCD
- 1) Map triggers and accommodations. List the top compulsions and ways you currently accommodate (e.g., answering the same question 10 times). Choose two accommodations to replace with supportive alternatives this week. Start where success is most likely.
- 2) Pick two love languages to pilot. Attach them to ERP goals (e.g., Words of affirmation + Quality time during Saturday exposure). Pilot, debrief, repeat.
- 3) Measure and adjust. Track minutes of exposure, number of reassurance requests, mood (0–10), and relationship closeness (0–10). Review weekly. Data beats memory when anxiety is loud—and it keeps arguments shorter.
Common pitfalls (and fixes)
- Pitfall: “Kindness equals reassurance.” Fix: Validate feelings, not fears. Offer calm presence while declining repeat reassurance. Most couples stumble here first.
- Pitfall: Turning love languages into new rituals. Fix: Vary timing and format; don’t use them to neutralize anxiety. If it starts to feel compulsory, change it up.
- Pitfall: Going it alone. Fix: Loop in a therapist trained in ERP. Partners can join sessions to fine-tune boundaries. A Harvard-affiliated program once called this “outsourcing the referee” for a reason.
When to get more support
If symptoms escalate, daily life is being consumed by compulsions (more than an hour a day is a common clinical threshold), or ROCD themes intensify, seek ERP-focused care. Meta-analyses show ERP/CBT yield large, durable symptom reductions for many adults. This is treatable; help sooner tends to work better.
Image alt: Couple practicing ERP and connection using the 7 Love Languages for OCD
Bottom line
The 7 Love Languages for OCD won’t replace therapy, but they can make love feel steadier—warmer, clearer, more effective—by reducing accommodation, reinforcing ERP, and keeping values at the center. Used with care, they let you say “I’m here” without saying “I’ll do your rituals.” That balance is the work.
Summary
Use the 7 Love Languages for OCD to pair compassion with science: validate feelings, reduce reassurance loops, and align care with ERP. Start with two languages, set boundaries, and track progress. Treatment works—love can help it stick. Bold step: schedule a partner check-in this week and pick one supportive action each.
References
- National Institute of Mental Health (NIMH). Obsessive-Compulsive Disorder. https://www.nimh.nih.gov/health/statistics/obsessive-compulsive-disorder-ocd
- Olatunji BO, Davis ML, Powers MB, Smits JAJ. Cognitive-behavioral therapy for OCD: A meta-analysis of treatment outcome and moderators. Clin Psychol Rev. 2013;33(8):1178-1191. https://pubmed.ncbi.nlm.nih.gov/24128603/
- Calvocoressi L, et al. Family accommodation in obsessive–compulsive disorder. Am J Psychiatry. 1995;152(3):441-443. https://pubmed.ncbi.nlm.nih.gov/7793464/
- Storch EA, et al. Family accommodation in pediatric OCD. J Clin Child Adolesc Psychol. 2007;36(2):207-216. https://pubmed.ncbi.nlm.nih.gov/17632200/
- Boeding SE, et al. Family accommodation in adults with OCD: Clinical correlates. J Anxiety Disord. 2013;27(5):456-463. https://pubmed.ncbi.nlm.nih.gov/23810139/
- Doron G, Derby D, Szepsenwol O. Relationship obsessive–compulsive disorder (ROCD): Conceptualization and treatment. J Obsessive-Compulsive Relat Disord. 2014;3(2):169-180. https://www.sciencedirect.com/science/article/pii/S2211364914000237
- Egbert N, Polk D. Speaking in Love Languages: A test of Chapman’s five love languages. J Soc Pers Relat. 2006;23(4):553-567. https://doi.org/10.1177/0265407506065983
Ready to try this together? Share this article with your partner, pick two love languages to pilot, and book an ERP-informed session this month.
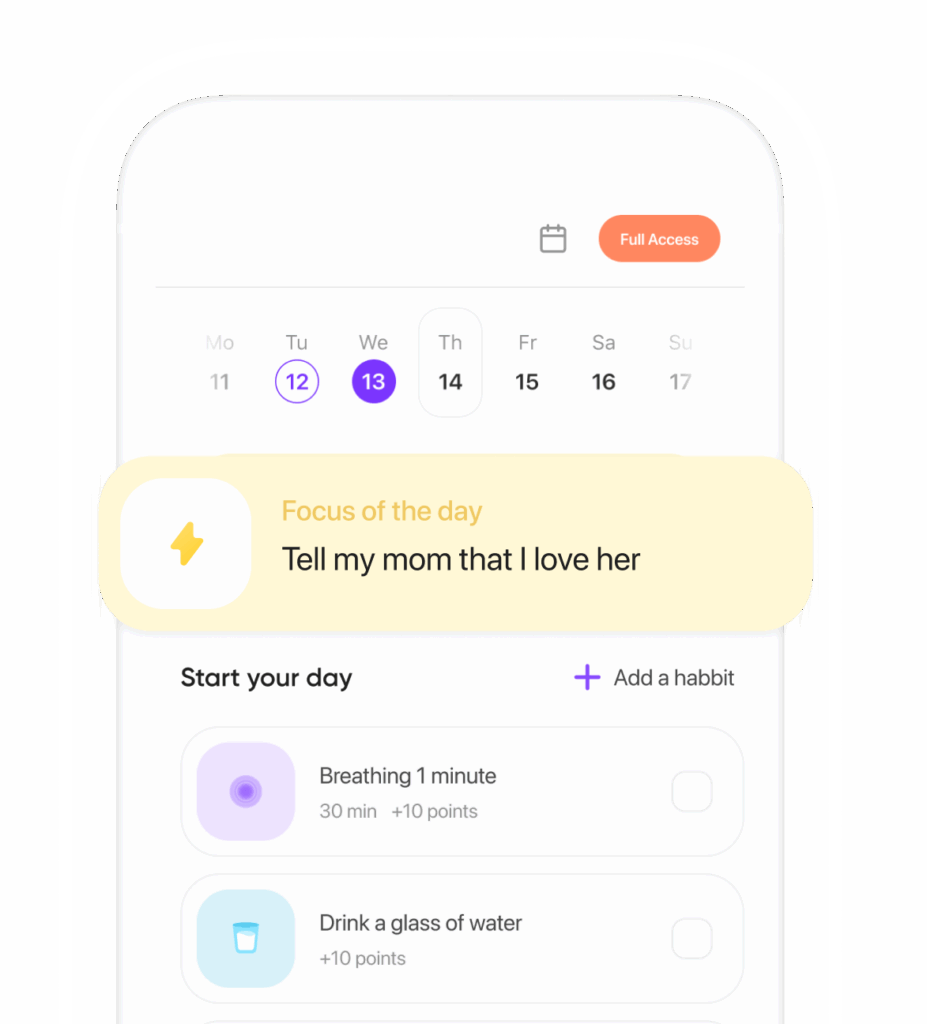
Ready to transform your life? Install now ↴
Join 1.5M+ people using AI-powered app for better mental health, habits, and happiness. 90% of users report positive changes in 2 weeks.