Table of Contents
- Overview
- Why 7 Love Languages for Panic Attacks Can Help
- How to Use 7 Love Languages for Panic Attacks, One by One
- Words of affirmation
- Quality time
- Physical touch
- Acts of service
- Receiving gifts
- Digital connection
- Shared experiences
- Build Your Personal Plan Using 7 Love Languages for Panic Attacks
- Safety notes
- Image suggestion
- The bottom line
- Summary
- References
Overview
When your heart sprints and thoughts go grainy, it helps to have a plan that feels human—warm, repeatable, and close at hand at 2 a.m. or on a crowded train. That’s the promise of the 7 Love Languages for Panic Attacks: a practical, science-shaped way to translate care—yours or a partner’s—into actions that bring the body back down. Pair them with simple grounding and paced breathing, and you have a toolkit you’ll actually use when it counts.
Why 7 Love Languages for Panic Attacks Can Help
- Panic disorder touches roughly 4–5% of people over a lifetime, and many more will meet a sudden surge at least once. The evidence, over decades, points to cognitive behavioral therapy and exposure as the most effective treatments for reducing panic symptoms and fear of sensations. It remains the backbone of care (Hofmann et al., 2012; Craske & Barlow, 2008).
- Love languages aren’t a clinical model, but the mechanisms under them are familiar to science: social support buffers stress physiology (Heinrichs et al., 2003), affectionate touch and even hand-holding can dial down neural threat responses (Coan et al., 2006), and slow, paced breathing with attention-anchoring grounding techniques shifts the nervous system toward safety (Meuret et al., 2008). The long-running Harvard Study of Adult Development has said much the same in broader terms: relationships protect health over the long haul. In plain terms, connection calms; I’d argue it does so faster than most people expect.
- Pairing each “language” with a brief breath practice and a grounding cue creates multiple on-ramps back to steady. In 2020, The Guardian reported a sharp rise in downloads of breathwork and meditation apps as anxiety spiked; by 2021, just-in-time digital prompts had become routine for many. The principle holds—more cues, fewer barriers.
How to Use 7 Love Languages for Panic Attacks, One by One
Words of affirmation
- Self: Script a short, factual line you can say out loud: “This is a panic surge. It will peak and pass. I can breathe and ride it.” Keep it on your lock screen or a wallet card. What do you most need to hear when fear surges? Use that—no fluff.
- Partner/friend: Reflect what you see without drama: “I’m here. Your body is alarmed, but you’re safe. Breathe with me: in for 4, out for 6.” Keep your pace steady, your tone low.
- Why it helps: Calm, accurate self-talk interrupts catastrophic misinterpretation—central in panic—while paced breathing helps correct over-breathing. In practice, the plainer the words, the better; jargon rarely soothes.
Quality time
- Self: Create a 10-minute “recovery window” after a surge—sit with your pet, step outside, or take a slow walk while noticing five things you see, four you feel, three you hear. It’s simple, repeatable, and kind.
- Partner/friend: Offer undistracted presence. Match breaths, count exhales together to 6–8 seconds, or guide a slow body scan. No multitasking, no pep talks—just be there.
- Why it helps: Co-regulation—safely syncing with another’s calm—reduces reactivity, and focused attention trims worry loops. I’ve seen quiet presence outperform clever tips more often then not.
Physical touch
- Self: Place one hand on your chest and one on your belly; feel the lower hand rise with each slow inhale. Try a cool splash to the face or hold an ice cube to the wrist for 10–20 seconds to trigger a brief “dive” reflex.
- Partner/friend: With consent, hold hands or offer firm, steady pressure to shoulders or mid-back. Keep your voice low and slow, your movements predictable.
- Why it helps: Touch can lower cortisol and perceived threat; face cooling can nudge heart rate down via vagal pathways. When touch is welcome, it’s one of the fastest levers we have.
Acts of service
- Self: Pre-pack a “panic kit”: water, mint gum, a soft cloth, a scent you like, and a card with your steps (breathing, grounding, who to text, when to seek care).
- Partner/friend: Handle small logistics during/after a surge—open a window, fetch water, silence notifications, walk with them to fresh air. Offer to practice drills together 2–3 times a week for five minutes.
- Why it helps: Reducing decisions in the moment preserves bandwidth and reinforces effective habits. Practical help beats platitudes every single time.
Receiving gifts
- Self: Use a weighted lap blanket, a cooling face mist, or noise-canceling earbuds with a preloaded 6-breaths-per-minute track. A small stone or mala can anchor your hands and focus.
- Partner/friend: Give a care bundle that fits their plan—CO2-normalizing breath app, a soothing playlist, peppermint or ginger candies (useful if nausea hits), and a note with their affirmations.
- Why it helps: Tangible items cue skills and make them easier to start; deep pressure and paced-breathing aids can lower arousal. I’m partial to weighted blankets—quiet, heavy, effective.
Digital connection
- Self: Create a panic “favorites” folder on your phone: a 1-minute box-breath video, a timer set to 4-in/6-out, a grounding checklist, and a text template to request support now—right now.
- Partner/friend: Send brief coaching texts on rough days: “Timer on for 1 minute: in 4, out 6. I’m here. Text ‘done’ when finished.” If agreed, do a live two-minute breathing call.
- Why it helps: Just-in-time mobile nudges can reduce symptoms and boost follow-through. Used sparingly, tech becomes a lifeline, not a crutch.
Shared experiences
- Self: Plan graded outings with a buddy to gently face triggers (caffeine, warm rooms, crowds). Start small, stay until anxiety rises and falls, then leave—classic exposure, done kindly.
- Partner/friend: Be a calm coach—no safety crutches, lots of steady presence. Debrief afterward: “What went better? What did you learn?” Keep it factual, not evaluative.
- Why it helps: Supported exposure rewires threat learning—the gold standard for panic. It’s uncomfortable—and it’s how the fear map changes.
Build Your Personal Plan Using 7 Love Languages for Panic Attacks
- Identify your top two languages and map one breathing exercise and one grounding technique to each. Simple beats clever.
- Write a 5-line crisis script (affirmation, breath count, 5-4-3-2-1 grounding, who to text, when to seek care).
- Practice daily when calm for 3–5 minutes; skills stick better outside crisis. Track what works in a notes app or paper log. If attacks are frequent or disabling, seek CBT with exposure; it’s highly effective. A 2021 APA brief echoed what clinicians already know: repetition builds confidence.
Safety notes
- Rule out medical issues if symptoms are new or different.
- Touch is opt-in only. If trauma is present, prioritize agency.
- If you have suicidal thoughts, seek immediate help.
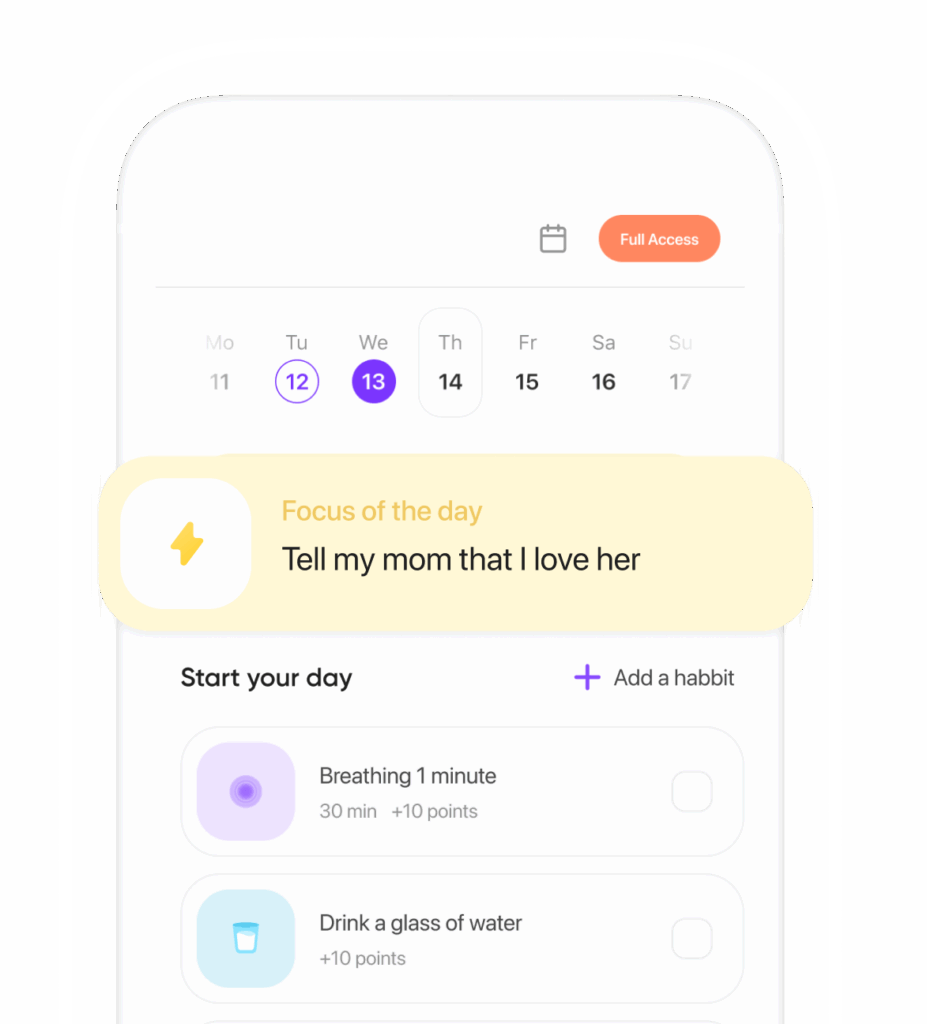
Image suggestion
Alt: 7 Love Languages for Panic Attacks grounding kit: A small pouch with a breathing card, mints, smooth stone, earbuds, and a calming spray on a bedside table.
The bottom line
The 7 Love Languages for Panic Attacks turn caring into concrete steps: soothing words, steady presence, consented touch, practical help, supportive tools, digital coaching, and brave shared practice. Paired with breathing and grounding, they become a reliable, evidence-aligned plan you can reach for when panic surges—and recover faster, with more confidence.
Summary
Panic is intense but temporary; your body can relearn safety. Using the 7 Love Languages for Panic Attacks, match affirming words, time, touch, service, gifts, digital support, and shared exposure with simple breathing and grounding to regulate faster. Practice when calm, personalize your kit, and track wins. Build your two-language plan today and share it with a support buddy.
References
- Hofmann, S. G., et al. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research. https://doi.org/10.1007/s10608-012-9476-1
- Craske, M. G., & Barlow, D. H. (2008). Panic disorder and agoraphobia. In: Clinical Handbook of Psychological Disorders. https://doi.org/10.1037/0003-066X.44.3.450 (overview)
- Meuret, A. E., et al. (2008). Targeting abnormal physiology in panic disorder: Carbon dioxide–enhanced therapy. Journal of Psychiatric Research. https://doi.org/10.1016/j.jpsychires.2008.02.003
- Coan, J. A., et al. (2006). Lending a hand: Social regulation of the neural response to threat. Psychological Science. https://doi.org/10.1111/j.1467-9280.2006.01730.x
- Heinrichs, M., et al. (2003). Social support and oxytocin interact to suppress cortisol and subjective responses to stress. Biological Psychiatry. https://doi.org/10.1016/S0006-3223(03)00465-7
- Holt-Lunstad, J., et al. (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine. https://doi.org/10.1371/journal.pmed.1000316
- Firth, J., et al. (2017). The efficacy of smartphone-based mental health interventions for anxiety. World Psychiatry. https://doi.org/10.1002/wps.20472
Ready to transform your life? Install now ↴
Join 1.5M+ people using AI-powered app for better mental health, habits, and happiness. 90% of users report positive changes in 2 weeks.