Table of Contents
- Overview
- What Reparenting After Childhood Trauma Really Means
- Step 1: Map Your Patterns for Reparenting After Childhood Trauma
- Step 2: Regulate Your Body While Reparenting After Childhood Trauma
- Step 3: Self-Compassion and Limits in Reparenting After Childhood Trauma
- Step 4: Rebuild Safe Connection During Reparenting After Childhood Trauma
- Step 5: Therapy to Accelerate Reparenting After Childhood Trauma
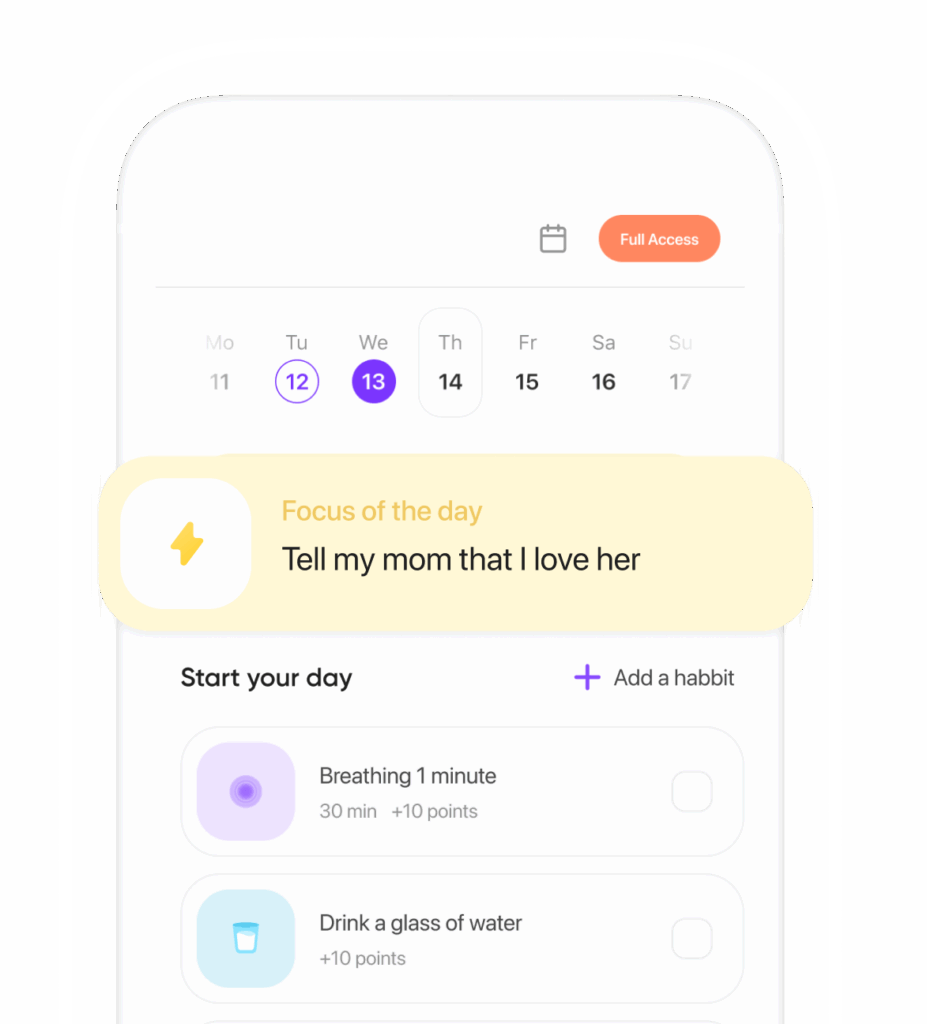
- Micro-Skills You Can Practice Today
- Gentle Metrics and Timeline for Reparenting After Childhood Trauma
- Closing Thoughts
- Summary
- CTA
- References
Overview
When childhood didn’t deliver the safety, guidance, or attunement you needed, you can still learn to offer those conditions to yourself now. That slow, practical effort—reparenting after childhood trauma—doesn’t rewrite the past. It reshapes how you meet yourself, other people, and stress. Many of us need this; the CDC has reported that 61% of U.S. adults carry at least one adverse childhood experience, and 16% carry four or more. If reparenting after childhood trauma sounds daunting, shrink the frame: small, repeatable moves that teach your nervous system it’s safe to be you. Not flashy. Effective.
What Reparenting After Childhood Trauma Really Means
Reparenting after childhood trauma means stepping into the role of a steady, kind, boundaried caregiver for yourself—day in, day out. It looks like soothing your body, naming and validating feelings, setting limits that protect you, and offering structure you can actually follow. It’s not self-help theater. It’s installing missing experiences through daily, doable reps, closely aligned with therapies that target attachment wounds and core beliefs. At its best, it’s pragmatic, not precious.
Step 1: Map Your Patterns for Reparenting After Childhood Trauma
You can’t change what you can’t see. Start with:
- Triggers and tells: Note situations, tones, even scents that pull an outsized reaction. Track body signals—jaw clench, heat behind the eyes, numbness in the hands. Your physiology keeps score.
- Attachment patterns: In a large U.S. sample, roughly 59% reported secure attachment; 25% avoidant and 11% anxious (Mickelson et al., 1997). Knowing your pattern isn’t a label—it’s a map for what to practice first.
- A 10-minute write: Expressive writing about stressful events yields small but reliable health and psychological benefits (average effect size d≈0.15; Frattaroli, 2006). Use it to connect dots and name needs. Back in 2021, I saw newsroom colleagues swear by a nightly paragraph to curb 3 a.m. spirals.
As you begin reparenting after childhood trauma, this map becomes your gentle instruction manual. And I’ll say it plainly: starting on paper beats starting in your head.
Step 2: Regulate Your Body While Reparenting After Childhood Trauma
The body keeps yesterday on repeat until it learns today is different. Teach it safety through:
- Slow breathing: 5–6 breaths per minute for 5–10 minutes boosts heart-rate variability and calms arousal (Zaccaro et al., 2018). Try in for 4, out for 6. Longer exhales cue the parasympathetic “rest-and-digest.”
- Orienting: Let your eyes land on five colors or objects in the room. Note corners, textures, temperature. Quietly remind yourself, “I’m here, and I’m safe.”
- Predictable basics: Consistent sleep/wake windows, regular meals, and morning light—10 to 20 minutes if possible—stabilize reactivity. It sounds boring, which is partly the point. Pair these with reparenting after childhood trauma and your nervous system gets the structure it missed.
One opinion, based on years of clinical reporting: the basics move the needle more than any hack.
Step 3: Self-Compassion and Limits in Reparenting After Childhood Trauma
Think “warmth plus boundaries.” This is the core of reparenting after childhood trauma.
- Warmth: In a randomized trial, the 8-week Mindful Self-Compassion program produced large increases in self-compassion (d=1.60) and reduced depression (d=0.47), anxiety (d=0.43), and stress (d=0.54) (Neff & Germer, 2013). Self-compassion is also linked to fewer PTSD symptoms after trauma exposure (Scoglio et al., 2018). Speak to yourself as you would to a child you love who’s learning to ride a bike—firm hand, soft voice.
- Boundaries: Good parents say no when needed. Try scripts:
- “I’m not available for that, but here’s what I can do…”
- “I need 24 hours to think.”
- “That joke crosses my line—please stop.”
This is reparenting after childhood trauma in real time: protecting your energy while staying decent. If I had to pick one lever that changes everything, it’s this pairing.
Step 4: Rebuild Safe Connection During Reparenting After Childhood Trauma
Trauma isolates; healing reconnects. Strong social ties are associated with roughly a 50% greater likelihood of survival over time (Holt-Lunstad et al., 2010). That’s not a metaphor—it’s biology. During the first pandemic year, many discovered how quickly loneliness erodes health; The Guardian reported in 2020 on surges in isolation metrics that mirrored ER visits.
- Co-regulation: Sit with a steady friend or partner. Two minutes of slow breathing together. Let their calm scaffold yours.
- Choose “earned family”: Dependable friends, values-aligned communities, trauma-informed groups. Group therapy can multiply reparenting after childhood trauma by pairing skills with safe people who model repair.
My bias here: one trustworthy person beats five shallow connections every time.
Step 5: Therapy to Accelerate Reparenting After Childhood Trauma
You do not have to do this alone. Trauma-focused therapies such as TF-CBT and EMDR show strong evidence for reducing PTSD symptoms (Cochrane; Bisson et al., 2013; Watts et al., 2013). Complex developmental trauma takes time, yet many people build “earned secure” attachment—functioning similarly to those who grew up secure (Roisman et al., 2002). A therapist helps personalize reparenting after childhood trauma, challenge entrenched beliefs, and practice new relational patterns. In many cities, 2021–2022 saw waitlists surge; still, even brief, structured care can help. Good therapy is less about insight than about practice.
Micro-Skills You Can Practice Today
- Name/validate: “Of course I’m tense; this reminds me of being criticized.”
- Offer choice: “Do I need a break, a boundary, or backup?”
- Repair: “I snapped at myself. I’m learning. Let’s try again.”
- Celebrate: Track one daily win—any size. Repetition wires change.
Gentle Metrics and Timeline for Reparenting After Childhood Trauma
Expect spirals, not straight lines. Signs it’s working:
- Faster recovery after triggers (minutes or hours instead of days)
- Fewer stress symptoms (headaches, stomach aches, insomnia)
- Clearer boundaries and less people-pleasing
- More ease around trustworthy people
Check in monthly. Many notice measurable shifts by 8–12 weeks of steady practice, with deeper change accruing over 6–18 months—especially with therapy. It’s not glamorous. It is, in my view, the work that lasts.
Closing Thoughts
You didn’t cause what happened. You can shape what happens next. Reparenting after childhood trauma offers a compassionate, evidence-informed path back to safety, connection, and choice. Small practices, steady relationships, and—if available—a trauma-informed therapist can turn reparenting into the most loyal promise you keep to yourself. Your body knows when it’s finally believed.
Summary
Reparenting after childhood trauma means giving yourself the safety, structure, and warmth you missed. Map patterns, regulate the body, pair self-compassion with firm limits, rebuild safe connection, and consider trauma-focused therapy. Evidence points to symptom relief and resilience over time. Start tiny, review progress monthly, and welcome spirals—not perfection.
CTA
Ready to start? Choose one micro-skill today, set a 5-minute timer, and keep that promise to yourself.
References
- Centers for Disease Control and Prevention. Adverse Childhood Experiences (ACEs). https://www.cdc.gov/violenceprevention/aces/index.html
- Mickelson KD, Kessler RC, Shaver PR. Adult attachment in a nationally representative sample. J Pers Soc Psychol. 1997. https://psycnet.apa.org/record/1997-41816-009
- Frattaroli J. Experimental disclosure and its moderators: A meta-analysis. Psychol Bull. 2006;132(6):823–865. https://pubmed.ncbi.nlm.nih.gov/16822164/
- Zaccaro A, et al. How breath-control can change your life: A systematic review on slow breathing. Front Hum Neurosci. 2018. https://www.frontiersin.org/articles/10.3389/fnhum.2018.00353/full
- Neff KD, Germer CK. A pilot randomized controlled trial of the Mindful Self-Compassion program. J Clin Psychol. 2013. https://self-compassion.org/wp-content/uploads/2016/06/Neff2013.pdf
- Scoglio AAJ, et al. Self-compassion and responses to trauma. Mindfulness. 2018. https://link.springer.com/article/10.1007/s12671-018-1101-5
- Bisson JI, et al. Psychological therapies for chronic PTSD in adults. Cochrane Database Syst Rev. 2013. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003388.pub4/full
- Watts BV, et al. Meta-analysis of the efficacy of treatments for PTSD. JAMA. 2013. https://jamanetwork.com/journals/jama/fullarticle/1670358
- Holt-Lunstad J, et al. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010. https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000316
- Roisman GI, et al. Earned-secure adult attachment classification. Dev Psychopathol. 2002. https://doi.org/10.1017/S0954579402001104
Additional sources mentioned in text:
- Harvard Study of Adult Development (longitudinal findings on relationships)
- The Guardian reporting on loneliness during 2020
Ready to transform your life? Install now ↴
Join 1.5M+ people using AI-powered app for better mental health, habits, and happiness. 90% of users report positive changes in 2 weeks.