How to Ease Childhood Trauma Flashbacks can feel overwhelming, and for many people they arrive without warning. The room shifts, the body jolts, old scenes play as if now. Still—there are skills that can pull you back to the present with some speed and dignity. This guide blends step-by-step tools with research and lived clinical reporting so you can practice safely, build a simple plan, and recognize when extra help is the wiser move. One view, borne out by years in newsrooms and clinics: the basics work better then most apps.
Table of Contents
- How to Ease Childhood Trauma Flashbacks: fast grounding when it hits
- Build your plan for How to Ease Childhood Trauma Flashbacks
- Therapies and tools that show How to Ease Childhood Trauma Flashbacks
- Body-based adjuncts for How to Ease Childhood Trauma Flashbacks
- Smarter self-talk during How to Ease Childhood Trauma Flashbacks
- When to get urgent help
- Summary
- CTA
- References
How to Ease Childhood Trauma Flashbacks: fast grounding when it hits
When your body alarms, get oriented first and lower arousal second. The simplest tools often beat the fancy ones.
- Name and locate: “This is a flashback. I am safe now in [location], and it’s [date].” Brief, clear labeling interrupts the spiral; cognitive reappraisal like this sits at the core of effective PTSD treatments (Ehlers & Clark, 2000). It sounds small. It isn’t.
- 5-4-3-2-1 senses: Identify 5 things you see, 4 feel, 3 hear, 2 smell, 1 taste. Catalog them out loud if you can. Sensory grounding competes with intrusive imagery and returns you to the here-and-now—desk, window, clock, breath.
- Paced breathing: Inhale for 4 seconds, exhale for 6, for about 2–3 minutes. Emphasize the out-breath. Longer exhalations increase heart-rate variability and dial down the sympathetic surge (Zaccaro et al., 2018). A timer on your phone helps.
- Temperature shift: Run cool water over your hands and face or hold an ice pack for 30–60 seconds. That brief cold engages the dive reflex, slowing heart rate and softening intensity. Bathroom sink works fine; you don’t need gear.
- Gentle movement: Press your feet into the floor. Stretch your calves. Try bilateral tapping—alternate taps on shoulders or thighs—to re-anchor in your body. It looks simple because it is.
Practice these when you’re calm. Muscle memory matters; in a spike, you’ll reach for what’s already familiar. My take: two techniques, used consistently, beat eight you forget.
Build your plan for How to Ease Childhood Trauma Flashbacks
Personalize tools and supports before you need them. The unglamorous work pays back, often quietly.
- Track triggers: Note cues (smells, dates, tones) and early signs (numbing, tunnel vision). The CDC reported in 2019 that more then 60% of adults carry at least one adverse childhood experience, and pattern awareness often prevents spirals (CDC, 2019). A plain notebook works as well as any app.
- Write a safety script: Two or three lines you can read aloud mid-flashback. Example: “I’m remembering, not reliving. I can breathe, look around, and text X for support.” Keep a copy on your phone and one on paper. It’s your voice—make it sound like you.
- Create a sensory kit: Mints, textured fabric, a grounding stone, a calming playlist, and a photo that reliably signals safety. Small, portable, boring. That’s the point.
- Co-regulation: Choose 1–2 people you can message, and tell them exactly how to help (e.g., “remind me of the date and ask me to breathe”). Social support consistently predicts better PTSD outcomes (Ozer et al., 2003). One good helper beats a crowd.
- Aftercare: Hydrate, eat a protein-rich snack, and set up sleep. Sleep disturbance intensifies intrusions; stabilizing sleep reduces next-day reactivity (Germain, 2013). A 20-minute walk the same afternoon can help that night.
Therapies and tools that show How to Ease Childhood Trauma Flashbacks
If flashbacks are frequent, disabling, or stealing hours from your week, trauma-focused therapies work. In my view, they remain the backbone of care.
- Trauma-focused CBT/CPT/PE: Strong evidence shows these reduce intrusions and avoidance; they’re first-line in the NICE PTSD guideline (NICE NG116, 2018). An AHRQ review found large, durable symptom improvements (Cusack et al., 2016). A Harvard-affiliated summary reached similar conclusions in 2021.
- EMDR: As effective as trauma-focused CBT for many adults; helps reconsolidate traumatic memories so they intrude less (Chen et al., 2014). Many patients describe fewer and shorter flashbacks after a structured course.
- Medications: SSRIs (sertraline, paroxetine) can reduce overall PTSD symptoms for some. For nightmares that fuel daytime flashbacks, prazosin may help certain people, though a large veteran trial saw no overall benefit on PTSD symptoms (Raskind et al., 2018). A clinician can help match options to your profile and history.
Access can be a barrier—The Guardian reported in 2022 that waits for trauma therapy lengthened in parts of the U.K.—so asking about group formats or telehealth may shorten the path to care.
Body-based adjuncts for How to Ease Childhood Trauma Flashbacks
Add nervous-system regulators alongside therapy. Not a cure-all; useful levers.
- Yoga and interoceptive practices: In a randomized trial, 52% of women doing trauma-sensitive yoga no longer met PTSD criteria vs 21% of controls (van der Kolk et al., 2014). These practices can reduce intensity and speed of flashbacks. Gentle, repeated, predictable.
- Breath/HRV training: Slow, coherent breathing boosts vagal tone and emotion regulation (Zaccaro et al., 2018). Aim for 5–6 breaths per minute for about 10 minutes daily. A metronome or paced-breath app can guide you, but a ticking analog clock does too.
Smarter self-talk during How to Ease Childhood Trauma Flashbacks
- Validate and orient: “My brain is trying to protect me. I can look for three blue objects and feel my feet.” This is not indulgent; it’s tactical.
- Shrink the image: Imagine the scene as a small, distant picture; add a transparent “safety filter.” A common cognitive therapy trick—reduce vividness, reduce grip. If it feels contrived, that’s fine; repetition gives it teeth.
When to get urgent help
Seek immediate support if flashbacks trigger urges to harm yourself, you feel out of control, or you can’t reorient. In the U.S., call or text 988 (24/7). In the U.K. and Ireland, Samaritans are available at 116 123. If outside these regions, see your country’s crisis line via the International Suicide Prevention wiki or contact local emergency services. Asking early is not weakness; it’s judgment.
You’re not weak for needing help; you’re learning a new way to relate to old pain. Practicing these skills, building your plan, and using evidence-based care can reclaim your attention, your sleep, and your days. One calm hour is a foothold; several make a week.
Summary
Easing childhood trauma flashbacks hinges on rapid grounding, a personalized plan, and proven therapies. Use breath, orientation, and sensory tools in the moment; prepare scripts, kits, and supports; and consider TF-CBT or EMDR. Address sleep and add body-based practices for resilience. Boldly ask for help early. If one door is closed, try the next—persistence matters.
CTA
Ready to build your plan? Bookmark this, assemble your kit today, and schedule a consult with a trauma-informed therapist this week.
References
- Centers for Disease Control and Prevention (2019). Vital Signs: Adverse Childhood Experiences. https://www.cdc.gov/mmwr/volumes/68/wr/mm6844e1.htm
- Ehlers, A., & Clark, D. (2000). A cognitive model of PTSD. Behav Res Ther. https://pubmed.ncbi.nlm.nih.gov/10802471/
- Ozer, E. et al. (2003). Predictors of PTSD: Meta-analysis. J Consult Clin Psychol. https://pubmed.ncbi.nlm.nih.gov/12795570/
- NICE Guideline NG116 (2018, updated). PTSD: diagnosis and management. https://www.nice.org.uk/guidance/ng116
- Cusack, K. et al. (2016). Psychological Treatments for Adults With PTSD. Ann Intern Med. https://www.acpjournals.org/doi/10.7326/M15-2489
- Chen, Y.-R. et al. (2014). EMDR vs CBT in adult PTSD: Meta-analysis. PLoS One. https://pubmed.ncbi.nlm.nih.gov/25180382/
- Raskind, M. et al. (2018). Trial of Prazosin for PTSD in Veterans. N Engl J Med. https://pubmed.ncbi.nlm.nih.gov/29414272/
- Germain, A. (2013). Sleep disturbances as hallmark of PTSD. Sleep Med Rev. https://pubmed.ncbi.nlm.nih.gov/23639538/
- Zaccaro, A. et al. (2018). Breath-control and emotion. Front Hum Neurosci. https://www.frontiersin.org/articles/10.3389/fnhum.2018.00444/full
- van der Kolk, B. et al. (2014). Yoga as adjunctive treatment for PTSD. J Clin Psychiatry. https://pubmed.ncbi.nlm.nih.gov/25004196/
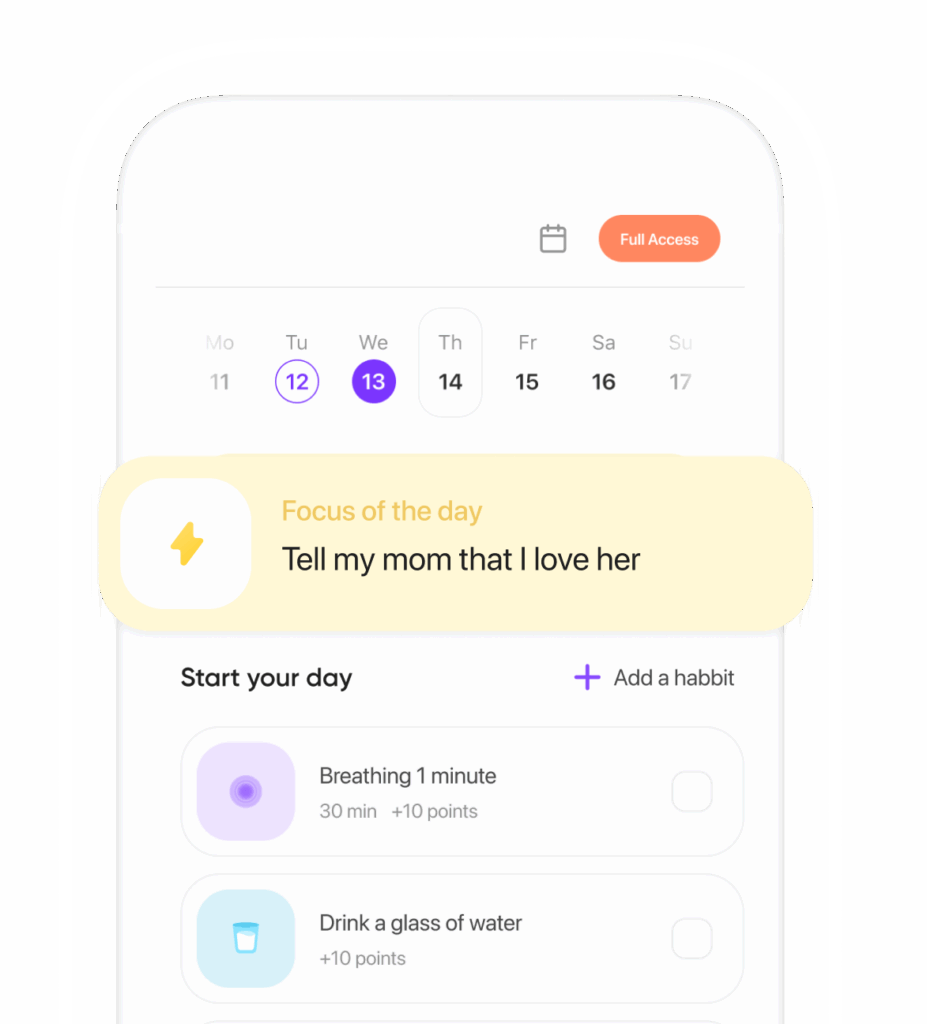
Ready to transform your life? Install now ↴
Join 1.5M+ people using AI-powered app for better mental health, habits, and happiness. 90% of users report positive changes in 2 weeks.