If you live with post‑traumatic stress, sleep can feel like another battlefield. Meditation for PTSD nightmares offers a practical, science‑backed way to reduce nighttime fear, reclaim rest, and rebuild safety. Up to 50–70% of people with PTSD have recurrent nightmares that worsen insomnia, anxiety, and daytime functioning—yet targeted practice can change that pattern. Back in 2015, a JAMA trial with veterans found mindfulness reduced symptom burden and improved quality of life. It’s not a cure; it’s a tool. In my view, it’s one of the more humane tools we have.
[Image alt: meditation for PTSD nightmares bedtime routine]
Table of Contents
- Why meditation for PTSD nightmares can work
- Before you start: safety first
- A 4‑part practice: meditation for PTSD nightmares nightly protocol
- Weekly progression and tracking
- Troubleshooting
- When to get more help
- Closing thoughts
- Summary
- References
Why meditation for PTSD nightmares can work
- It calms hyperarousal. PTSD primes the nervous system to stay on high alert. Mindfulness training reduces limbic reactivity and strengthens prefrontal regulation, which supports steadier emotion control and startle recovery. Randomized trials—like the 2015 JAMA study—show mindfulness-based stress reduction (MBSR) decreases PTSD symptom severity and improves quality of life in veterans. It won’t erase memories, but it changes your relationship to them. The evidence isn’t perfect, but it’s stronger then skeptics assume.
- It improves sleep regulation. Meditation can reduce sleep disturbance and nighttime rumination, two key drivers of nightmares. In 2015, Harvard‑affiliated researchers reported that a brief mindfulness program outperformed standard sleep‑hygiene education for older adults with sleep complaints, which signals it can ease pre‑sleep arousal that feeds trauma dreams. To me, that’s the quiet power here—less drama, more regulation.
- It pairs well with proven nightmare tools. Imagery Rehearsal Therapy (IRT)—the gold‑standard behavioral treatment—rescripts the storyline of a nightmare while awake. Layering IRT with meditation for PTSD nightmares may boost adherence by lowering anxiety during practice. Clinically, the combination often travels farther than either alone.
Before you start: safety first
Trauma‑sensitive practice keeps you within a tolerable window. Before using meditation for PTSD nightmares, set up:
- A grounding plan (cold water, weighted blanket, scent, pet).
- An anchor (breath, feet on the floor, or the feeling of your hands).
- A “stop” rule: if distress exceeds 7/10, open your eyes, orient to the room, and switch to movement or a soothing task.
- Professional support if nightmares escalate. Medications like prazosin have mixed evidence; talk with your clinician about fit and timing. You can use meditation for PTSD nightmares alongside therapies such as CBT‑I, IRT, EMDR, or prolonged exposure. A brief consult up front can save weeks of trial and error—worth it.
A 4‑part practice: meditation for PTSD nightmares nightly protocol
Total daily time: 20–30 minutes. This routine is deliberately light; in my experience, people stick with what feels doable on hard days.
1) Daytime nervous‑system reset (3–5 minutes)
- Slow breathing: Inhale 4, pause 1, exhale 6–8, pause 1. Five rounds.
- Why: Slow breathing reduces sympathetic drive and improves vagal tone, supporting calmer nights.
- Tip: Label sensations (“warm,” “tight,” “buzzing”) without judgment. Even two micro‑sessions help when you later use meditation for PTSD nightmares. In plain terms: breathe out longer than you breathe in—simple, not easy.
2) Early‑evening body scan (10–15 minutes)
- Lie down or sit. Sweep attention from toes to scalp, noticing pressure, temperature, and tension. Let each exhale soften one small area.
- Why: Body scans increase interoceptive awareness and downshift arousal. Longitudinal work suggests mindfulness practice is associated with decreased amygdala activation.
- If overwhelmed, narrow your focus to neutral zones (heels, hands). You’re still using meditation for PTSD nightmares by teaching your body a predictable wind‑down. Consistency beats intensity here.
3) Pre‑sleep rescripting + mindful imagery (8–10 minutes)
- Write a 2–6 sentence “new version” of your nightmare with a safe, empowering turn (e.g., a locked door, a helper appears, a bright light). Keep it plausible to you.
- Sit, breathe, then read the script slowly three times, visualizing as vividly as is comfortable. When fear arises, note “fear is here,” feel your anchor, continue gently.
- Why: IRT reduces nightmare frequency and distress and improves sleep. Adding mindful acceptance reduces avoidance that can block IRT. This is the core of meditation for PTSD nightmares—meeting the story calmly while shaping a new ending. If you feel silly doing this, you’re not alone; do it anyway.
4) Middle‑of‑night reset (5 minutes)
When you wake from a nightmare:
- Orient: Name five things you see, four you feel, three you hear.
- Temperature cue: Splash cool water or hold a chilled object.
- Counted breathing: 4‑in/6‑out for 10 breaths.
- Kindness phrase: “This was a memory; I’m safe right now.” Place a hand on your heart.
- Option: One minute of loving‑kindness (“May I feel safe. May I rest.”). Compassion practices can increase positive affect, which counters threat memory networks.
These steps are a mini‑dose of meditation for PTSD nightmares that interrupts the fear spiral and helps you re‑enter sleep. As newsrooms have reported—The Guardian among them—many veterans describe the “3 a.m. dread.” This is how you thin it out, night by night.
Weekly progression and tracking
- Keep a simple nightmare log: date, intensity (0–10), control (0–10), rescripting used (Y/N), and sleep quality (0–10).
- Aim for five days/week of practice. Expect small wins first (faster calm after waking, briefer nightmares) within 2–4 weeks; frequency often shifts later.
- If a specific image is “sticky,” use 3–5 minutes of eyes‑open mindful observation of that image during the day, then reapply your rescript. This extends meditation for PTSD nightmares beyond bedtime so it’s less charged at night.
I favor paper logs over apps—it’s boring, yes, but the pen slows the mind in its favor.
Troubleshooting
- “Meditation makes it worse.” Shorten sessions to 2–3 minutes, practice eyes open, or switch to movement‑based mindfulness (slow walking). Return to rescripting once arousal drops.
- “I can’t visualize.” Write the rescript and read it out loud. Record your voice and play it gently. You’re still doing meditation for PTSD nightmares by engaging attention and intention.
- “I fall asleep during practice.” Great—let the body take the rest. Run a shorter script earlier in the evening.
If you miss a night, skip the guilt. The only rule that matters is the one you’ll keep.
When to get more help
- Nightmares intensify for two weeks despite practice.
- You use alcohol/cannabis regularly to sleep.
- Suicidal thoughts emerge. Reach out to a clinician or crisis resource immediately.
Combining IRT or CBT‑I with meditation for PTSD nightmares often yields the best and fastest results. A brief course—six to eight weeks—can change the trajectory more then many expect.
Closing thoughts
You deserve sleep that restores, not reopens wounds. With steady, trauma‑sensitive practice, meditation for PTSD nightmares can calm your body, change the story, and help you wake with more control and less fear. Start small, track progress, and get support when needed—your nervous system can learn safety again. I’ve seen people reclaim their nights; it’s painstaking, and it’s possible.
Summary
Meditation for PTSD nightmares works by lowering hyperarousal, improving sleep regulation, and pairing with rescripting to change threat memories. Use a four‑part routine: daytime breathing, evening body scan, mindful IRT, and a middle‑of‑night reset. Track weekly, adjust for safety, and combine with therapy when needed. Boldly protect your rest.
Start tonight: pick one step, set a 10‑minute timer, and try it.
References
- Polusny MA et al. Mindfulness-Based Stress Reduction for Veterans With PTSD: A RCT. JAMA. 2015.
- Black DS et al. Mindfulness Meditation and Improvement in Sleep Quality. JAMA Intern Med. 2015.
- Gallegos AM et al. Mindfulness-based interventions for PTSD: systematic review and meta-analysis. Clin Psychol Rev. 2017.
- Nappi CM et al. A review of nightmares in PTSD. Sleep Med Rev. 2012.
- Casement MD, Swanson LM. Imagery rehearsal therapy: a review. Psychol Trauma. 2012.
- Hölzel BK et al. Mechanisms of mindfulness meditation. Perspect Psychol Sci. 2011.
- Jerath R et al. Physiology of long pranayamic breathing. Breathe. 2015.
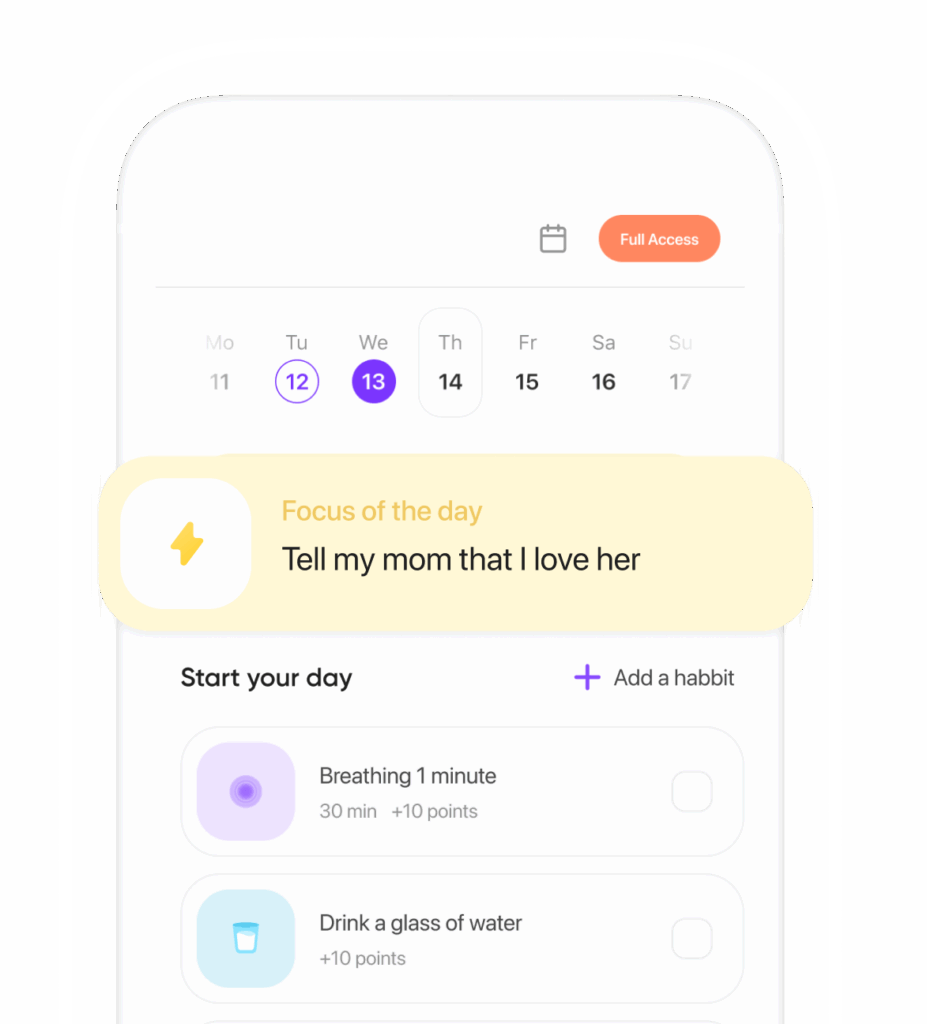
Ready to transform your life? Install now ↴
Join 1.5M+ people using AI-powered app for better mental health, habits, and happiness. 90% of users report positive changes in 2 weeks.