If you promised yourself you’d “do it differently” and still end most days overwhelmed, you’re not an outlier—you’re typical. Back in 2019, CDC data estimated 61% of U.S. adults had at least one adverse childhood experience (ACE) and roughly 1 in 6 reported four or more. Those early hits raise the odds of stress reactivity and relationship strain in adulthood. What follows are seven signs childhood trauma can shape day‑to‑day parenting—and practical ways to change course. Not perfectly. Just steadily.

Table of contents
- 7 signs childhood trauma affects parenting
- 1) Big reactions to small behaviors
- 2) Hypervigilance about safety and control
- 3) Hot-cold boundaries
- 4) Feeling numb, detached, or checked out
- 5) Your child’s crying or defiance triggers the past
- 6) Conflict-heavy co‑parenting or difficulty trusting others with your child
- 7) You see patterns repeating despite your best intentions
- How childhood trauma affects parenting—and what helps
- Why this matters for your child—and for you
- Closing thoughts
- Summary
- Ready to start?
- References
7 signs childhood trauma affects parenting
1) Big reactions to small behaviors
A whine. A slammed door. Milk on the floor. Your body floods the zone before your mind has a say. It’s not weakness; trauma history sensitizes the threat-detection system, which can prime adults for harsher or inconsistent responses. That moment when you think, I’m overreacting—your nervous system likely got there first. In my view, the unfair part is how automatic it feels.
Try this: Name the state out loud (“I’m triggered”), then exhale slowly—three rounds, longer out than in. Wait ten seconds before speaking. Training regulation skills has been shown to lower parenting stress and reduce harshness over time.
2) Hypervigilance about safety and control
Every climb looks like an ER visit in the making. Routines become rigid, because the unknown is louder than the known. Brains wired by adversity often scan for danger first, comfort second. The paradox: too much control can amplify conflict and anxiety in kids who need room to practice manageable risk. My take: safety and autonomy are not enemies; they’re a matched set.
Try this: Design “safe autonomy” zones—a couch they’re allowed to scale with clear rules, a step stool by the sink. Swap “Be careful!” for a coaching cue: “Find your balance… now check your feet.”
3) Hot-cold boundaries
You aim for warmth. Then fatigue hits and you swing—gentle one hour, shutdown or strict the next. Parents with ACEs are more likely to struggle with consistency, and across multiple meta-analyses, harsher discipline links to poorer outcomes in most measured domains. Consistency beats intensity. And yes, that’s harder on thin sleep. My opinion: simple, repeatable scripts are worth more than grand speeches.
Try this: Script one neutral boundary per repeat trigger. For hitting: “I won’t let you hit. Hands on your lap.” For throwing: “Balls outside; blocks stay on the floor.” Use the same words every time—tone light, limit firm.
4) Feeling numb, detached, or checked out
Closeness can feel costly when your own history coded closeness as risky. During your child’s big feelings, you might go quiet, far away, or vaguely frozen. Attachment research finds that unresolved trauma in caregivers raises the likelihood of disorganized attachment in infants. Repair, not perfection, is the hinge. My view: warmth delivered in small, steady doses travels farther than grand gestures.
Try this: Practice “micro-connection.” Thirty-second hugs. One full minute of eye contact while passing a snack. A gentle hand squeeze during a tantrum’s tail end. Frequent, brief repairs change the day’s emotional average.
5) Your child’s crying or defiance triggers the past
A tantrum detonates and suddenly you’re back there—panic, shame, a flash of something old. The body remembers faster than language. Triggers can hijack your response before your thinking brain is online. That’s not character; that’s conditioning. My view: planning for rupture is more realistic than pretending it won’t happen.
Try this: Set a “tap out” plan with a co‑parent or friend—one word you can say to step away. Keep a grounding kit nearby: cold water on wrists, paced breathing (in 4, out 6), a time stamp (“It’s 2026; this is my child, not my parent”). Then re-enter when steady enough to connect.
6) Conflict-heavy co‑parenting or difficulty trusting others with your child
When betrayal sits in your past, control battles can bloom in the present—over nap routines, pickups, who decides what. Maternal ACEs correlate with higher parenting stress, and stress spills into the couple dynamic and support networks. My perspective: structure is mercy when trust is thin.
Try this: Use brief, structured check-ins: What worked today? What was hard? One plan for tomorrow. Keep it under ten minutes. Skill-based co‑parenting—clear roles, shared language—reduces reactive back-and-forth.
7) You see patterns repeating despite your best intentions
Intergenerational transmission of risk is well documented; parents maltreated in childhood show higher odds of passing on vulnerability. But it’s risk, not destiny. Protective skills interrupt the loop. My view: upstream tweaks—done daily—change more than downstream willpower ever could.
Try this: Track one repeating pattern for two weeks (say, yelling at bedtime). Identify the earliest cue (tight shoulders at 6:45 p.m., the rush to finish dishes), and intervene there—turn on calming music at 6:30, start the routine ten minutes earlier, set a one-line limit before the spiral begins.
How childhood trauma affects parenting—and what helps
-
Build a trauma-informed plan
- Privately note your ACEs. It’s not a verdict; it’s a map for where to add support.
- Stabilize the basics: sleep, steady meals, movement, sunlight. A regulated body steadies the parent who lives inside it.
-
Evidence-based supports
- Child-Parent Psychotherapy (CPP) has randomized-trial evidence for reducing child behavior problems and caregiver PTSD in trauma-exposed dyads.
- Parent-Child Interaction Therapy (PCIT) yields large effects on disruptive behavior and boosts positive parenting across multiple reviews.
- Mindfulness-augmented parent programs show reductions in parenting stress and improvements in emotion regulation. The Harvard Center on the Developing Child has long underscored how such “serve-and-return” skills build resilience.
-
Attachment repairs beat perfection
- You’ll miss cues. A lot. Research on parent–infant interaction shows mismatch is common—the key is the circle back: “I got loud. I’m sorry. Let’s try again.” The Guardian once called this “the power of a good apology”—I agree.
-
Practical daily tools
- The 90-second rule: stress hormones crest quickly; anchor your breath until the wave passes.
- Narrate your regulation: “My voice is tight; I’m going to sip water.” Modeling teaches without a lecture.
- Pre-commit scripts for hot spots (meals, bedtime): one calm limit + one choice + one empathy line.
-
When to seek extra help
- If flashbacks, nightmares, or daily impairment show up, trauma-focused CBT or EMDR can help. Treating trauma symptoms often improves parental sensitivity as a downstream effect.
Why this matters for your child—and for you
Higher ACE counts in mothers are linked to increased odds of toddler developmental and behavior challenges. Yet supportive, consistent caregiving buffers risk—again and again in the data. Each time you notice how childhood trauma affects parenting and make a small repair, you’re not just managing a moment. You’re revising a storyline, protecting your child while healing parts of yourself that waited years for steady care.
Closing thoughts
Children don’t need flawless childhoods. They need good-enough care, offered reliably, with repairs when we miss. The fact that you’re reading about how childhood trauma affects parenting is a crack in the old pattern already. Keep going. Measured change, repeated often, is how families turn.
Summary
Many Millennial and Gen Z parents carry ACEs that shape stress responses, boundaries, and attachment. The seven signs above can help you spot when childhood trauma affects parenting. Evidence-based tools—CPP, PCIT, mindfulness, and day-to-day repairs—can interrupt intergenerational risk. Small, steady changes do the heavy lifting.
Ready to start?
Bookmark this, pick one tool to practice today, and consider a consult with a trauma-informed therapist.
References
- Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of Adverse Childhood Experiences, 2015–2017. MMWR. 2019;68(44):999–1003. https://www.cdc.gov/mmwr/volumes/68/wr/mm6844a1.htm
- Madigan S, Cyr C, Eirich R, Fearon RMP, Ly A, Rash C. Maternal history of maltreatment and infant disorganized attachment: A meta-analysis. Dev Psychopathol. 2019;31(1):83–98. https://pubmed.ncbi.nlm.nih.gov/30246619/
- Gershoff ET, Grogan-Kaylor A. Spanking and child outcomes: Old controversies and new meta-analyses. J Fam Psychol. 2016;30(4):453–469. https://pubmed.ncbi.nlm.nih.gov/27055181/
- Lieberman AF, Van Horn P, Ghosh Ippen C. Toward evidence-based treatment: Child-Parent Psychotherapy with preschoolers exposed to marital violence. J Am Acad Child Adolesc Psychiatry. 2005;44(12):1241–1248. https://pubmed.ncbi.nlm.nih.gov/16327784/
- Thomas R, Zimmer-Gembeck MJ. Parent-Child Interaction Therapy: An evidence-based treatment for child behavior problems. Clin Psychol Rev. 2012;32(6):383–395. https://pubmed.ncbi.nlm.nih.gov/22658963/
- Coatsworth JD, Duncan LG, Greenberg MT, Nix RL. Changing parents’ mindfulness, child management skills and relationship quality with their youth: Results from a randomized pilot intervention. J Child Fam Stud. 2015;24(2):348–359. https://pubmed.ncbi.nlm.nih.gov/26062266/
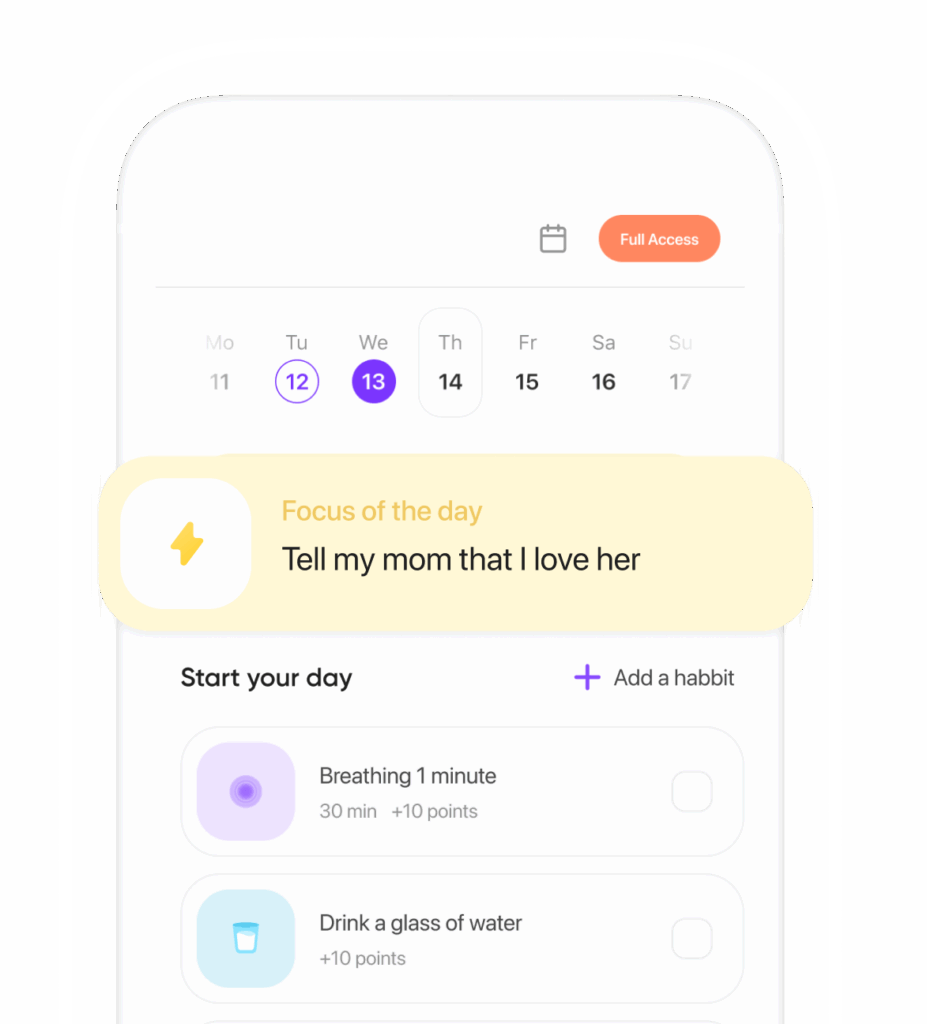
Ready to transform your life? Install now ↴
Join 1.5M+ people using AI-powered app for better mental health, habits, and happiness. 90% of users report positive changes in 2 weeks.