When depression flattens energy, mood, and motivation, love can feel like it can’t get through. Yet it can—if it’s delivered in small, credible ways. Using the 7 love languages for depression gives you practical, research-aligned tools to reconnect with care, for yourself and with people who want to help. Not grand gestures. Signals—repeated, specific, gentle. These cues reduce isolation, nudge activity, and quiet stress systems that have gone on high alert.
Why this approach works: supportive relationships lower depression risk and improve outcomes; behavioral activation (tiny, meaningful actions done consistently) rivals many therapies in effect size; and touch, encouragement, and everyday routines help regulate the body’s stress response. The WHO’s 2023 factsheet reminds us how common depression is worldwide; what it does not say outright is how much small, steady support matters. Below, how to use the 7 love languages for depression—on your own and with someone who cares.
Table of Contents
- What are the 7 Love Languages for Depression?
- How to Use 7 Love Languages for Depression—Solo and With Others
- 1) Words of Affirmation
- 2) Quality Time
- 3) Acts of Service
- 4) Physical Touch
- 5) Receiving Gifts
- 6) Shared Experiences/Play
- 7) Space and Autonomy
- Build a 2‑Week Micro‑Plan Using the 7 Love Languages for Depression
- Safety, Boundaries, and When to Get Help
- Troubleshooting the 7 Love Languages for Depression
- Summary
- CTA
- References
What are the 7 Love Languages for Depression?
- Words of Affirmation: compassionate, reality‑based encouragement.
- Quality Time: present, low‑pressure time together.
- Acts of Service: practical help that lightens the load.
- Physical Touch: safe, consent‑based touch that soothes.
- Receiving Gifts: thoughtful tokens that spark interest or ease.
- Shared Experiences/Play: simple activities that reawaken interest and joy.
- Space and Autonomy: protective boundaries that honor capacity.
How to Use 7 Love Languages for Depression—Solo and With Others
1) Words of Affirmation
- If you’re supporting yourself: Write a two‑to‑three line note that pairs validation with a cue to act: “This is hard, and I’ve done hard things. I’ll take a 5‑minute walk.” Self‑affirmation dampens stress physiology and makes follow‑through more likely—backed by lab studies going back at least a decade. In my view, the key is believable words over pep‑talks.
- If you’re supporting someone: Offer specific, accurate praise plus collaborative language: “You answered my text during a rough morning—that’s strong. Want company for a 10‑minute stretch?” Keep tone warm and concrete. Vague cheerleading rarely lands when someone’s hurting.
2) Quality Time
- Self: Schedule “micro‑time” with yourself—10 minutes of sun on the stoop, a favorite podcast while folding laundry. Behavioral activation trials show that even tiny, planned activities lift mood when repeated. It’s the cadence that counts more then intensity.
- With others: Co‑work quietly, watch a short show, share a silent coffee. Time together without performance pressure has the best odds of helping. I’d take 12 quiet minutes over an elaborate night out, any day.
3) Acts of Service
- Self: Use the “one‑shelf rule.” Tidy one shelf, send one email, wash one dish. Completing small tasks builds momentum and reduces overwhelm—that’s the behavioral activation core.
- With others: Offer two options and let them choose: “I can book your appointment or drop off dinner—what helps?” Practical help and perceived support both link to lower depressive symptoms in large reviews. Specificity beats “Let me know if you need anything,” which often leaves people stranded.
4) Physical Touch
- Self: Try three minutes of hand or neck self‑massage, a weighted blanket, or a warm shower. Touch reduces cortisol and can raise oxytocin, supporting emotional regulation; massage and warmth are not luxuries here, they’re tools.
- With others: Ask first: “Would a hug help?” A brief hug or hand‑holding can dampen threat responses in the brain (Coan’s lab showed this years ago). In my experience, consented touch is most effective when brief and predictable.
5) Receiving Gifts
- Self: Assemble a low‑cost “mood kit” (tea, cozy socks, a favorite snack) or add a bright plant to the desk. Prosocial spending—even $5—has been shown to boost well‑being; gifting yourself small comforts is a cue for self‑compassion, not indulgence.
- With others: Tiny, thoughtful gifts beat big gestures: a pre‑cut fruit cup, bath salts, a preloaded transit card. Link the gift to an easy action (“This tea is for your morning window time.”). The goal is friction‑reduction, not surprise and spectacle.
6) Shared Experiences/Play
- Self: Two‑minute play breaks: a song‑and‑stretch, doodling, a short dance. Pleasure plus movement improves adherence to activity plans; it’s why people return to the things that feel good, not just “good for you.”
- With others: Short, low‑stakes activities—five‑minute walk, simple recipe, a small puzzle. Shared experiences reduce rumination and gently reactivate reward pathways central to depression. During 2020, when many of us lost routine, even brief shared rituals made a difference; that hasn’t changed.
7) Space and Autonomy
- Self: Set a “floor, not ceiling” plan: one non‑negotiable tiny task, then permission to rest. Autonomy supports motivation and guards against shame spirals. Personally, I’d rather you hit the floor daily than sprint once and crash.
- With others: Say, “I care and I’m here. If you need quiet today, I’ll check tomorrow at 5.” Honoring pacing is part of care. Predictability reduces social fatigue and, over time, builds trust.
Build a 2‑Week Micro‑Plan Using the 7 Love Languages for Depression
- Choose one language per day, rotate across the week.
- Keep actions 2–10 minutes.
- Pair each action with a cue (alarm, or habit stacking like “after brushing teeth”).
- Track with a simple checkmark. Consistency beats intensity—almost always.
Example week:
- Mon (Affirmation): Read your note + send yourself one text.
- Tue (Quality Time): 10 minutes of sun + call a friend for 5.
- Wed (Service): One‑shelf rule.
- Thu (Touch): Warm shower + lotion hands, slowly.
- Fri (Gift): Buy a $3 treat; gift a friend a coffee.
- Sat (Shared Play): 5‑minute walk—scan for three lovely things.
- Sun (Space): One small task, then rest without guilt.
Safety, Boundaries, and When to Get Help
- If energy is near zero, shorten actions further (60–120 seconds). That still counts. Start where your body is, not where you wish it were.
- If you have thoughts of self‑harm, call or text 988 (US) or use local crisis services. These practices help, but they don’t replace professional care.
- Therapy plus these practices is powerful; behavioral activation and CBT have strong evidence, and social support predicts better outcomes. A 2015 review on relationships and depression made that point plainly.
Troubleshooting the 7 Love Languages for Depression
- “I feel nothing.” Numbness is common. Keep actions tiny and regular; feelings often follow behavior, not the other way around. It’s slow—then sudden.
- “People don’t get it.” Share this article and name 2–3 ways they can help. Scripts reduce guesswork and reduce the burden of explaining when you’re tired.
- “I lose momentum.” Bundle with daily anchors (coffee, commute) and ask a buddy for a two‑line evening check‑in. Accountability works best when it’s light and kind.
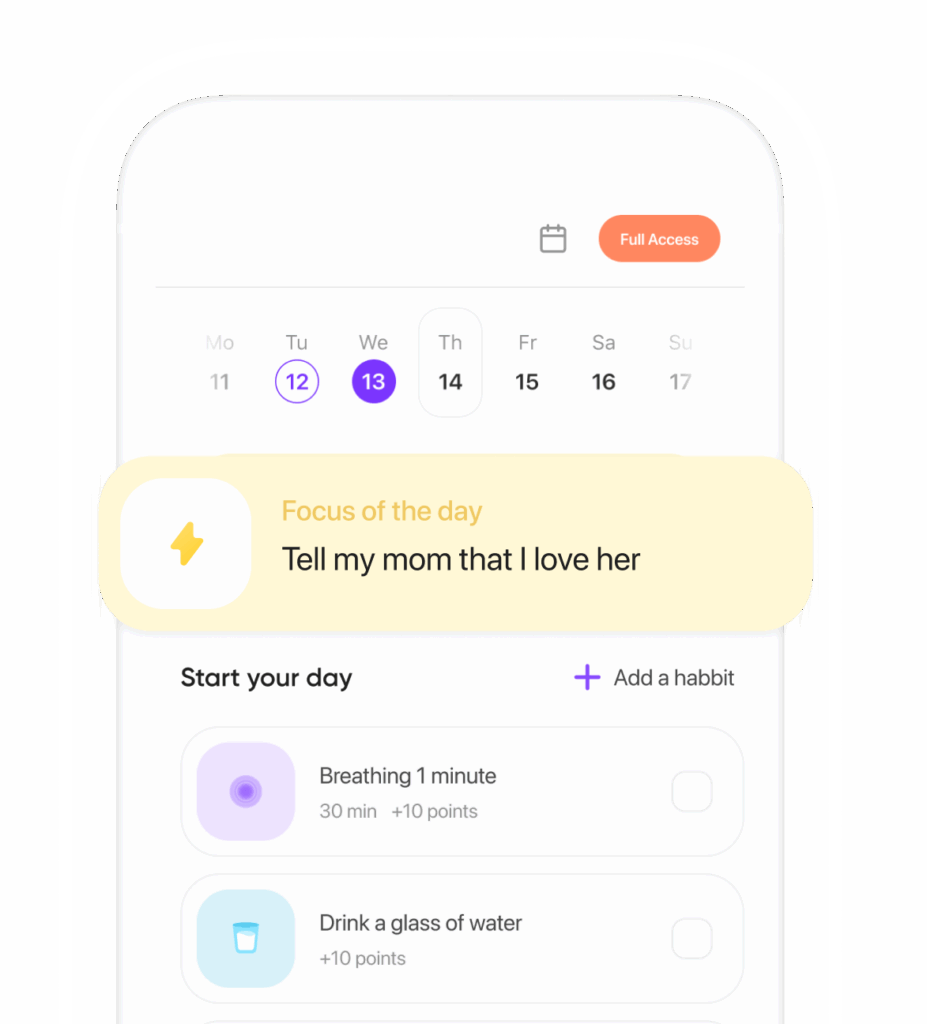
Image alt: Using the 7 love languages for depression—small daily acts, shared moments, and gentle routines that help mood heal
Closing thought: Love isn’t a cure. It is a lever. These seven channels turn care into doable, repeatable signals that shift biology, behavior, and belief—gradually, then all at once. Begin small, stay kind, and let consistency—not perfection—carry you.
Summary
The 7 love languages for depression translate connection into tiny, science‑backed actions—affirmations, time, service, touch, gifts, shared play, and space—that reduce isolation, activate behavior, and soothe stress. Use a two‑week micro‑plan, honor consent and autonomy, and pair with professional help when needed. Bold, small steps compound.
CTA
Screenshot this guide, pick today’s language, and set one 5‑minute action now.
References
- Coan, J. A., Schaefer, H. S., & Davidson, R. J. (2006). Lending a hand: Handholding and neural responses to threat. Social Cognitive and Affective Neuroscience, 1(1), 31–40.
- Cuijpers, P., van Straten, A., & Warmerdam, L. (2007). Behavioral activation treatments for depression: A meta‑analysis. Clinical Psychology Review, 27(3), 318–326.
- Dunn, E. W., Aknin, L. B., & Norton, M. I. (2008). Spending money on others promotes happiness. Science, 319(5870), 1687–1688.
- Field, T. (2010). Touch for socioemotional and physical well‑being: A review. Developmental Review, 30(4), 367–383.
- Ryan, R. M., & Deci, E. L. (2000). Self‑determination theory and the facilitation of intrinsic motivation, social development, and well‑being. American Psychologist, 55(1), 68–78.
- Santini, Z. I., Koyanagi, A., Tyrovolas, S., & Haro, J. M. (2015). The association between social relationships and depression: A systematic review. BMC Psychiatry, 15, 31.
- World Health Organization. (2023). Depression: Key facts. WHO Factsheet.
Ready to transform your life? Install now ↴
Join 1.5M+ people using AI-powered app for better mental health, habits, and happiness. 90% of users report positive changes in 2 weeks.